Weekly Update May 23, 2025
Protect MI Care and CMHA Medicaid advocacy resources
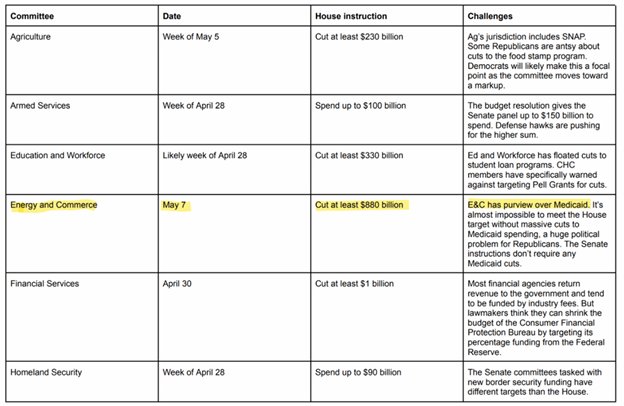
The Protect MI Care Coalition, a coalition in which CMHA is a member, recently issued a PMC statement on House passage of Medicaid cuts this morning from Protect MI Care Coalition chair, Monique Stanton, President and CEO of the Michigan League for Public Policy.
Congress Just Voted to Rip Health Care from More Than 500,000 Michiganders
Visit ProtectMICare.org to explore advocacy tools, news updates, and social media links.
This and other Medicaid protection advocacy materials are also posted on CMHA’s Advocacy Resources webpage.
Peer Recovery Coach provides powerful comments to close Medicaid Round Table
Nate Dunbar, a Peer Recovery Coach at the CMH Authority of Clinton, Eaton, and Ingham Counties, was beyond remarkable during Medicaid Round Table held in Lansing on May 21.
This town hall is the first of a series organized and sponsored by the Protect MI Care Coalition – the large and diverse coalition, of which CMHA is a member, designed to protect Medicaid against the cuts proposed by the federal administration and some in Congress.
Below is a news story on the Round Table including Nate’s photos and remarks. Impressive.
Michigan Advance: Michigan health advocates slam Trump bill cutting down Medicaid
An excerpt from a news story related to Nate’s comments:
Nate DUNBAR, a peer recovery coach who spoke during a roundtable, said the government was not listening to the people’s needs and Medicaid was a way to help people who couldn’t afford insurance.
“I resent people calling my fellow Michiganders waste and I resent people calling my fellow Michiganders abuse, and I resent people calling my fellow Michiganders fraud,” Dunbar said.
CMHA President named to Medicaid Advisory Group
Weekly Update readers may member that CMHA has been working with the MDHHS to recruit members for the Beneficiary Advisory.
The Beneficiary Advisory Council (BAC) is a newly forming statewide committee that will consist entirely of community members with lived experience. The primary role of the BAC will be to advise the Michigan Department of Health and Human Services (MDHHS) on policy development and effective administration of the Medicaid program. BAC members will have a formal voice in the decision-making process.
Recently, Craig Reiter, CMHA President, was recently named to this Advisory Council. Congratulations to Craig.
The Majority of Michiganders Oppose Medicaid Cuts, New Statewide Polling Shows
CMHA and a coalition of statewide associations and their members, recently commissioned a study of the views of Michiganders regarding Medicaid and the cuts being proposed, at the federal level, to the Medicaid program.
Below are excerpts from the press release announcing and providing the links to the results of that survey.
New statewide polling shows 83% of Michiganders want to see Medicaid spending increased or kept about the same as Congress considers cutting hundreds of billions of dollars from the Medicaid program, which would terminate healthcare for thousands of Michigan residents. The local results mirror national polls from the Kaiser Family Foundation, Modern Medicaid Alliance, and others that consistently show a lack of support for Medicaid cuts.
EPIC·MRA, with support from the Community Mental Health Association of Michigan, Michigan Association of Health Plans, Michigan Health & Hospital Association, Michigan Primary Care Association, and Protect MI Care, conducted the new statewide poll to determine where Michiganders stand on proposed cuts to Medicaid.
The full press release can be found here.
State & Federal Developments
Michigan 988 team announces report of 988 progress and impact
The Michigan 988 team recently issued the Quarterly Report.
This one-pager on the 988 Quality Metrics, which can be found here, covers a range of metrics including the number of 988 calls answered, the top reasons for calling 988, the average speed a call is answered, and other essential data.
Additionally, in honor of Mental Health Awareness Month, the 988 team has also shared materials that have been developed to raise awareness and support 988. This month highlights Michigan’s commitment to promoting awareness of and access to the 988 Suicide & Crisis Lifeline. You can find these resources in the 988 MiCAL Partner Toolkit and the SAMHSA Mental Health Awareness Month Toolkit.
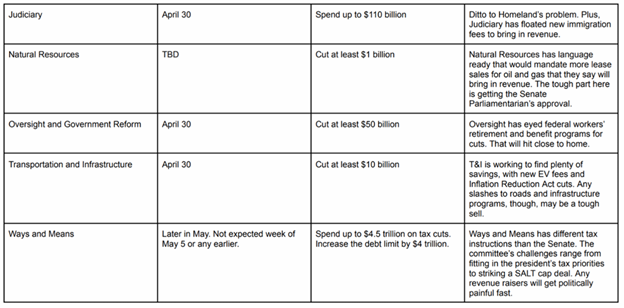
Hall Suggests More Cuts To Fund Roads Following May CREC Numbers
House Speaker Matt HALL (R-Richland Township) suggested today further cuts to “corporate handouts,” arts and cultural grants, the COVID-19 task force and an estimated 2,900 vacant government worker positions to make up the $320.2 million difference between January and May Consensus Revenue Estimating Conferences (CREC).
In January, CREC principals estimated that Fiscal Year (FY) 2026 would have $1.194 billion more to work with than they thought the previous year, but on Friday, principals estimated that number to be $320.2 million less.
Hall’s roads plan counted on about $600 million of the January CREC estimate, and today during a press conference gave suggestions on where the $320.2 million could be made up.
His suggestions include cutting remaining corporate handouts from the business attraction and community development fund for $100 million and the entrepreneurship ecosystem for $15 million, ending other programs like $22 million for the COVID-19 Task Force, $11 million for arts and cultural grants and $28 million for the Office of Global Michigan, and $150 million to eliminate 2,900 vacant government jobs that Hall called “phantom employees.”
All together, these cuts come to $326 million. Hall said the House budget will reverse the income tax hike, bring government workers back and fix local roads without increasing taxes.
Education, Sponsorship & Exhibition
Early Bird Registration Deadline May 30! CMHA 2025 Annual Summer Conference
Join us at the CMHA 2025 Annual Summer Conference for three days of connection, inspiration, and education in the behavioral health field. This year’s event features pre-conference institutes on leadership and board governance, powerful keynotes on resilience, advocacy, and lived experience, and a wide range of educational workshops covering CCBHC, autism services, youth and family supports, artificial intelligence, early psychosis, SDOH, opioid response, legislative advocacy, and more.
June 9–11, 2025 | Grand Traverse Resort – Acme, MI | Learn more and register!
Registration Open! 2nd Annual Michigan Substance Use Disorder Prevention Coalitions Conference
Join us for the 2025 SUD Prevention Coalitions Conference, a dynamic one-day event dedicated to empowering coalitions to excel as champions in substance use prevention. This year’s theme, Coalition C.H.A.M.P.S., highlights the critical components of effective coalition work: collaboration, health equity, advocacy, mobilization, perception, and sustainability. Whether you’re a seasoned coalition leader or new to prevention efforts, this conference will inspire and equip you to champion lasting change. Let’s come together to celebrate the power of collective action and ensure healthier, more resilient communities.
This conference is intended for prevention coalition leaders and members, prevention professionals, public health professionals, healthcare providers, and educators.
Exhibitor Opportunity! As a conference exhibitor, you will gain visibility throughout the day to promote your company’s brand, products, and services directly to approximately 200 attendees. Exhibitor Fee: $150. Your exhibitor fee includes one person at the exhibit table and entrance into all conference sessions and meals. Exhibitors register here!
June 24, 2025 | Riverfront Conference Center – Flint, MI | Learn more and register here!
Attention Nurses! ACT 201 RN Training Registration Open!
Join us for a training focused on the following areas: RN roles on ACT teams, common psychiatric diagnoses, psychiatric medications and side effects, and developing your nursing practice to manage self-care and avoid burnout. Participate in group discussions to share experiences, challenges, network with other nurses and earn Nursing CE credits.
June 17, 2025 | Treetops Resort in Gaylord, MI | Register now!
CMHA Events
To search all upcoming CMHAM events, including conferences, trainings and webinars click here.
Center for Mental Health Implementation Support (CMHIS)

CMHA has recently joined, as the Michigan partner, the Center for Mental Health Implementation Support (CMHIS) applies deep knowledge of how to sustainably implement effective mental health prevention, treatment, and recovery practices and programs to support organizations and systems in improving the lives of the people they serve.
CMHIS and its bi-regional Hubs can help your organization or system improve the delivery of mental health care by strategizing to overcome barriers and planning new program implementation from start to finish. CMHIS can help you map the course, navigate roadblocks, and provide support to ensure that the people who need it receive the excellent mental health care that providers always strive to deliver. CMHIS serves grantees funded by SAMHSA’s Center for Mental Health Services and organizations that oversee or directly provide mental health services. These organizations typically work with people with serious mental illness or serious emotional disturbance.
More information on CMHIS at: https://www.cmhisupport.org/
This project is supported by Grant Number SM090078 from the Substance Abuse and Mental Health Services Administration (SAMHSA) of the U.S. Department of Health and Human Services. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of SAMHSA/HHS or the U.S. Government.